
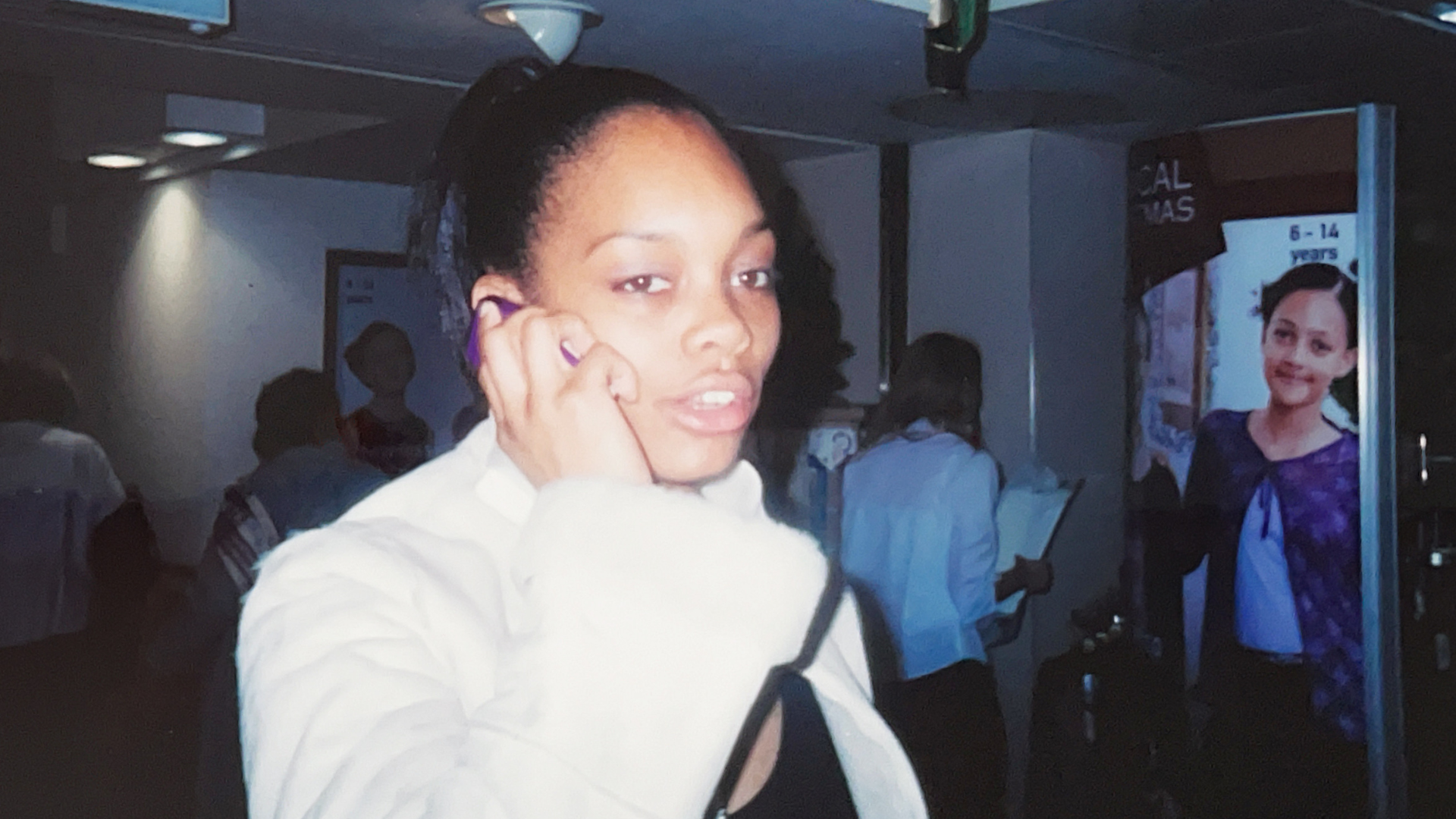
Vanessa Peat
28 October 2025
So many women live with pain that doesn’t have a name.
For years, I was one of them. I managed heavy bleeding and fatigue while trying to study, work, and raise a family, without understanding that these were signs of a condition that was yet to be diagnosed.
At university, I learned just how invisible women’s health challenges can be. Unless you have a formal diagnosis, the support you need often doesn’t exist.
University: Showing Up Without Being Seen
Being a student meant deadlines, lectures, and expectations that required attendance, absorption, and performance.
But when you’re dealing with heavy bleeding, constant pain, low iron, and fatigue, taking a “sick day” comes with educational consequences. Without a diagnosis, I couldn’t lean into the medical support I really needed. All I had was endurance.
I remember a friend who had been diagnosed with endometriosis. She could take time out of classes, and no one questioned it. I didn’t have that option, so I silently carried the weight of needing to be “fine.”
As a neurodivergent individual, I often processed information more slowly and in a different way than my peers. If I missed a lecture, catching up was often harder. Although a handwritten transcript service was available, it was very much down to how the individual provided the annotations rather than the full context. Relying on these alone made it difficult for me to absorb the information, as I ideally needed to be present in the room to take in the material visually and audibly, making the full use of being present felt conflicting when my productivity felt low.
And through all of this, I was a mother, caring for my children, as well as being a partner. When suffering in pain, the pressure to “just show up” became even greater; there was a lack of university support to help me step back when this all got too much, and I was fatigued. These compounding challenges often felt overwhelming, leading to further fatigue and overload.
In the background, I tried various contraceptives to manage symptoms: a coil, the implant, and pills. None solved the core problem. Some worsened mood or made bleeding unpredictable. One medication left me feeling even more low and exhausted. Following years of various failed interventions, I made the decision to have an endometrial laser ablation, which reduced my period pain, but still left me with heavy blood loss.
It was only through the insight of my partner (a trainee GP) that I realised something else was wrong.
This experience taught me something essential: knowing what’s normal for you, and having people who notice changes in you, can make all the difference.
Entering Work: Hidden Logistics, Unspoken Needs
When I first started seeking employment, the physical and logistical burden followed me.
- I wanted to know where restrooms were in every building.
- I had to plan escape routes for when bleeding overwhelmed me.
- I needed leeway to slip away, reset, or manage in silence.
- Some weeks, pain would sap me; other weeks I could function “normally.”
- Presenteeism, being there but not really there, was a real struggle.
All of this layered on top of neurodivergence: sensory overload, mental exhaustion, and emotional regulation challenges. It wasn’t just about pushing through aches; it was navigating a maze of hidden hurdles during the cycle of every single month.
The Wider Impact: Relationships, Self, and Stigma
When your body is at war, everything is collateral damage. Work relationships, friendships, and energy for family. These all begin to erode under pressure.
Because of the unspoken ‘it's normal’ narrative, this resulted in an internal, hidden emotional rollercoaster taking place.
Yet, when someone, family, friends, or colleagues noticed a change in me, such as looking paler due to iron depletion, or being lower in energy, and asked (gently, earnestly), that awareness became a lifeline.
I learned that creating “permission” to rest, to be open, is critical, yet many institutions, families, and workplaces don’t offer it. Instead, there is an unspoken narrative to hide, perform, keep silent and show up.
Creating safe spaces within workplaces is vital to break down this unspoken narrative and stigma, enabling individuals to be open and engage, seeking the support they need so they can thrive and not just try to survive.
What Science Says: Mood, Contraception & Invisible Connections

Research highlights the link between hormonal contraception and mood changes:
- Starting oral contraceptives is associated with an elevated risk of depressive symptoms, especially in the first two years (NCBI).
- Levonorgestrel-based IUDs can be linked with anxiety, depression, and sleep disturbances (NCBI).
- Evidence varies, and patient-level factors matter significantly (Pharmaceutical Journal).
For someone already coping with pain, heavy bleeding, and neurodivergent processing, these interactions can push you from “functioning” to “struggling.” To have support around decision points - starting, stopping, or changing your method of contraception is vital.
What Could Change: Workplace Support for Women’s Health
Large Corporations
Some larger organisations are beginning to lead the way in supporting women’s and reproductive health, demonstrating that workplace wellbeing must evolve to meet real, lived experiences.
For example:
- Deloitte has added a menopause plan within its private medical insurance and launched a menopause community to encourage open dialogue and peer support.
- KPMG provides access to menopause-trained GPs and nurses, offers flexible working arrangements, and runs monthly menopause cafés to create safe spaces for open discussion. It also has a menopause ambassador network and leadership training to ensure supportive, respectful workplace conversations.
These examples show what’s possible when large organisations move beyond awareness and into active, embedded policy change.

Small UK Companies
Even with limited budgets, support is possible:
- Flexible working arrangements can be put in place for women who have “difficult weeks” during their cycles.
- Wellness spaces, quiet rooms, or rest zones should be made freely available.
- Line manager training should include how to respond sensitively to women’s health needs.
- Scheduled wellness check-ins or “drop-in” chats could be embedded into workplace calendars.
Empathy, trust, and intentional design can make a bigger difference than expensive benefits.
For Universities
- Create policies that allow rest and flexibility without stigma.
- Normalise conversations about menstrual health, pain, and invisible disabilities.
- Embed support structures: mental health, occupational health, peer groups.
To women living with invisible pain
- Your experience is valid.
- Track what’s normal for you: symptoms, energy, mood.
- Seek advocates: friends, partners, clinicians, and don’t be afraid to reach out.
- Remember, contraceptive and medical decisions can affect mood and bleeding; they are all part of the wider picture.
Share stories like mine. The more visible these journeys are, the more we chip away at stigma and open up conversations that need to be heard.
In my next article, I’ll share how a GP visit revealed that chronic blood loss and low iron weren’t just something to endure, they were signs of something deeper. That finding led to a specialist referral and the start of a journey with the right team of experts. I’ll also share Dr Nicholas Peat’s perspective, both as my partner and as a medical professional.
